Ankle Fracture
Definition
An ankle fracture is a fracture of the inner and/or outer ankle of the foot. This is one of the most common bone fractures, most commonly affecting the outer ankle.
If one speaks of the ankle joint, one actually speaks of the "upper ankle joint". It is formed by three bones: Shin bone (= tibia), fibula and talus. Shinbone and fibula form a bony fork (= malleolus fork), which surrounds the anklebone in a U-shape. The upper ankle joint allows the foot to be raised and lowered.
The outer ankle is the joint process of the fibula, the inner ankle is the joint process of the tibia. A complex ligamentous apparatus ensures the stability of the ankle joint: outer ligaments, inner ligaments and anterior and posterior syndesmosis (= a very firm ligament connection between the tibia and fibula).
If, despite these relatively stable connections, a fracture of the ankle occurs, force transmission almost always causes injuries to the ligaments. In addition, both lower leg bones should be examined for additional bone fractures, especially if the inner ankle is involved throughout the entire process up to the knee. Sometimes a fracture of the fibula close to the knee joint (=Maisonneuve fracture) occurs as an accompanying injury.
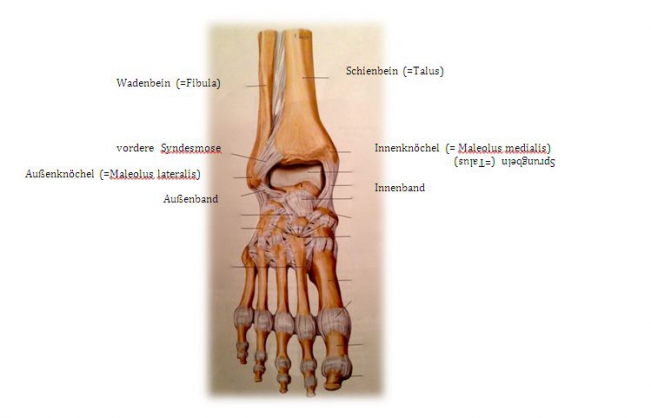
Fig.1) Anatomy of the upper ankle joint (from: Prometheus ®, MLP)
An ankle joint fracture is most often divided into three different forms by Weber's classification based on the height of the fracture at the fibula (outer ankle):
Weber A: Outer ankle fracture below syndesmosis (→ Syndesmosis always intact)
Weber B: Outer ankle fracture at syndesmosis level (→ Syndesmosis possibly injured)
Weber C: Outer ankle fracture above syndesmosis (→ Syndesmosis always injured)
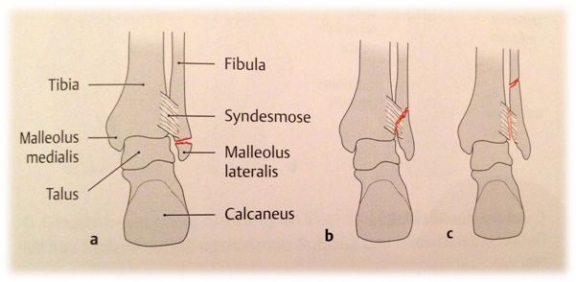
Fig. 2) Weber classification for ankle fractures (from: Prometheus ®, MLP)
In all three Weber forms, the inner ankle can also be broken or the inner ligament injured. However, this is not a criterion for this classification.
A combined fracture of the inner and outer ankle is referred to as a "bimalleolar ankle fracture" (see Fig. 3). If, in addition, the posterior lower tibia edge (=Volkmann's triangle) is broken, it is called "trimalleolar ankle fracture".
As with all fractures, a distinction is made between a closed fracture (= skin intact) and an open fracture (= open wound over the fracture). An open fracture always means a greater risk of infection, which can delay healing.
Typical causes
The ankle fracture is a typical sports injury. For example, when walking on uneven ground, in an abrupt change of direction or in the event of an incorrect occurrence, the foot can twist, which can cause an ankle fracture. But a fall from a low height can also cause a fracture of the ankle joint.
Symptoms
- aches
- swelling
- hematoma
- limited mobility
- load incapacity
- possible instability
- misalignment
- possible sensory disturbances in the foot
diagnostic
- Patient history: inquire the injury mechanism
- Physical examination:
√ Localization of the fracture by palpation
√ Testing the belt stability
√ Testing of vascular and nerve injuries
- X-rays: ankle joint and, if necessary, the entire lower leg
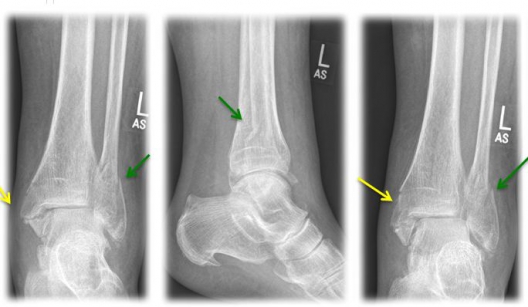
Fig. 3) "Bimalleolar ankle joint fracture" left x-rayed in 3 planes (a.p., lateral, internal rotation) with an internal ankle fracture (yellow arrow) and a spiral external ankle fracture (green arrow)
Computer tomography (= CT) if necessary: for questionable X-ray findings and for planning the operation
Magnetic resonance tomography (= MRT) if necessary: for clarification of ligament injuries as well as soft tissue and cartilage assessment
Treatment
In general, the type of bone fracture (open/closed, displaced/undisplaced) and the Weber classification determine the course of treatment.
In the case of a fracture with additional malpositioning of the upper ankle joint (= luxation fracture), the malposition should be corrected as early as possible by the emergency physician, if necessary at the accident site, in order to avoid pressure damage to the soft tissues (skin, nerves, vessels) caused by the bones.
- Indication for conservative therapy:
Procedure of choice for closed Weber A- and Weber B- fractures with non-displaced fracture and without syndesmosis injury
→ Relief boots (=Walker) for 6 weeks
- Indication for surgical therapy:
Procedure of choice for Weber C fractures, Weber A and Weber B fractures with displaced fracture and/or syndesmosis injury (for Weber B and/or open fractures and/or vascular and/or nerve injuries)
Method of choice in surgical therapy
- Internal ankle fracture: mostly use of cannulated screws or tension belt osteosynthesis
- Outer ankle fracture: usually insertion of a lag screw and a neutralization plate
- tape seam may be necessary if the inner tape can be folded out
- In case of syndesmosis injury, the insertion of an adjusting screw is necessary for 6 weeks to stabilize the syndesmosis.
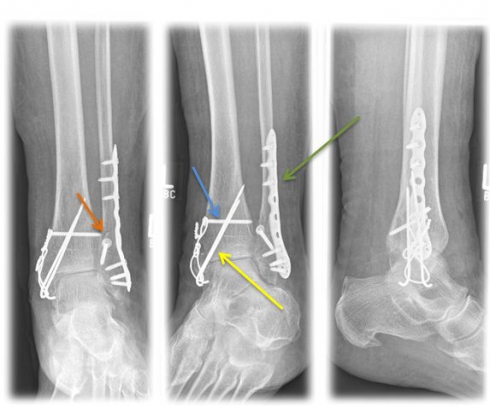
Fig. 4) Osteosynthetic treatment of a bimallel ankle fracture by means of tension belt osteosynthesis at the inner ankle (yellow arrow), neutralization plate (green arrow) and a traction screw (orange arrow) at the outer ankle as well as an adjusting screw (blue arrow).
Further Treatment
- Early physiotherapeutic exercise, load building and gait training depending on the fracture form, the stability of the osteosynthesis and the bone quality of the patient.
- clinical controls until full function of the ankle joint is regained
- regular x-ray checks to check the position of the fracture and the bony connective tissue (= bony consolidation)
- if an adjusting screw is inserted, this must be removed 6 weeks postoperatively, then a step-by-step build-up to full load is possible
- if the syndesmosis shows itself intact intraoperatively and an adjusting screw does not have to be used, the patient should partially load the joint with 20 kg for 6 weeks.
- sports activities are possible again after 3 to 6 months
Material removal
As a rule, the material can be removed at an individually determined time (depending on several factors, including the age of the patient, degree of activity of the patient, complaints), but at the earliest after 12 months postoperatively. It is possible to leave the osteosynthesis material in the body for a long time.






